While there may be no cure for this diverse disease, there are several treatment options that have come to light that may extend and improve the quality of life in Triple-Negative Breast Cancer patients.
Intro
Metastatic breast cancer, also called stage IV breast cancer, is a versatile disease that has spread to another part of the body, most commonly the liver, brain, bones, or lungs.
While there is no cure for metastatic breast cancer, there are treatment options that slow the cancer and improve quality of life. Many patients now live 10 years or more after a metastatic diagnosis. However, treatment options depend on a factor of things, such as receptor type.
Triple-Negative Breast Cancer
Normal breast cells have receptors — proteins that can attach to certain substances in the blood — to help them grow. Or, in the case of breast cancer cells, spread the disease. Breast cancer cells may have one, all, or none of these hormone receptors.
Triple-Negative Breast Cancer is a type of metastatic breast cancer that does not have any of the receptors such as ER, PR, or Her-2. Triple-Negative Breast Cancer has relatively high relapse rates and poor post-treatment outcomes. Fortunately, chemotherapy is still an effective option.
Traditional Chemotherapy & The Maximum Tolerated Dose
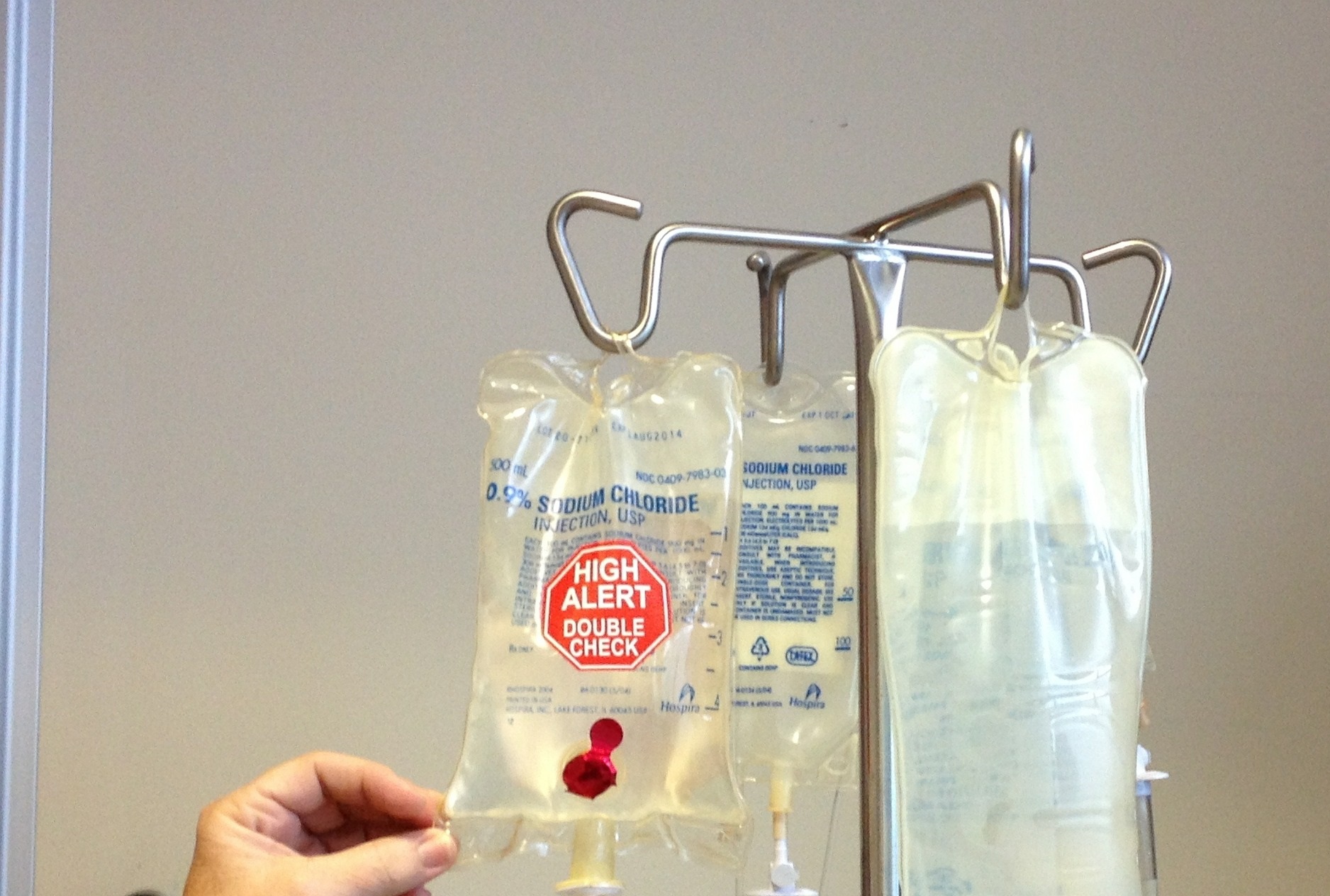
Chemotherapy falls under the category of cytostatic treatment, any substance that inhibits cell growth and division. Traditional use of this treatment revolves around the “maximum tolerated dose.”
Essentially, high doses of a chemotherapeutic agent are given at 2-4 week intervals. Chemotherapy does not specifically eliminate cancer cells, but rather disrupts the process of cell division.
Because of this, non-cancerous cells are damaged as well, leading to some severe side-effects. While the 2-4 week breaks from therapy allow the normal cells to recover and heal, they may also allow tumor cells to recover and develop resistance.
Side-Effects of Traditional Chemotherapy
When high doses of therapy are experienced, the non-cancerous cells undergoing damage cause many side-effects, some of which include:
Hair Loss: some or all hair may fall out within 2-4 weeks of starting chemotherapy. While hair will grow back around 4-6 weeks post-treatment, it may come in thinner than pre-treatment.
Nausea: Most patients feel sick and exhausted for a day or two after each chemotherapy treatment. It’s different for everybody, and doctors can provide a prescription to treat nausea.
Fatigue: Extreme tiredness, memory problems, or brain fog are common symptoms that may dissipate a few weeks after therapy ends.
To combat these side-effects, low doses of cytotoxic drugs are administered at shorter intervals. According to several studies, this low dose treatment may achieve tumor regression with minimal side-effects. This is termed Metronomic Chemotherapy.
Metronomic Chemotherapy & The Minimum Effective Dose
Low-Dose Metronomic Chemotherapy in metastatic breast cancer patients aims to prolong and improve quality of life. This concept relies on the continuous administration of chemotherapy at low doses and aims at targeting tumor endothelial cells specifically.
Endothelial cells line blood vessels and regulate exchanges between the bloodstream and the surrounding tissues. Cancer cells use the signals from endothelial cells to organize the growth of tumors.
During traditional chemo treatment breaks, the endothelial cells supplying the tumors with energy and growth signals are able to heal, developing new blood vessels to nourish cancer growth — a process known as angiogenesis.
Metronomic Chemotherapy aims to combat this by not providing enough time for endothelial cells to undergo angiogenesis. In this context, metronomic chemotherapy may offer the possibility of prolonged treatment with fewer side effects.
A number of “older” cytotoxic drugs, such as Capecitabine, have been tested in metronomic schedules. The majority of ongoing trials focus specifically on low-dose metronomic Capecitabine-based treatment. Recently, metronomic chemotherapy has been incorporated into the recommendations.
Understanding the Effectiveness of Metronomic Chemotherapy
In a recent study conducted by JAMA, eligible patients received Capecitabine at a dose of 650mg twice a day or standard chemotherapy for 1 year. Among women with early-stage triple-negative breast cancer who received treatment, low-dose Capecitabine therapy resulted in significantly improved 5-year disease-free survival.
A more recent study involved pretreated metastatic breast cancer with a combination of two cytotoxic drugs. Out of 48 patients, 1 patient had a complete response, meaning there is a disappearance of all signs of cancer.
Perraud et al. experimented with similar treatment options in 15 patients and found a clinical benefit rate of 46.7% with no serious toxicities. The effectiveness of this type of treatment has been long established.
Two decades ago, Calvert et al. used 50 mg of oral cytotoxic drugs for the first 14 days of 28-day cycles in 38 pretreated metastatic breast cancer patients. Eight of the patients had a partial response within 16 weeks.
In one other study from 2018, selected metastatic breast cancer patients with the triple-negative disease were given VEX as first-line therapy. The treatment was well tolerated and showed activity.
VEX therapy consists of vinorelbine 40 mg orally 3 times a week, cyclophosphamide 50 mg daily, and capecitabine 500 mg 3 times a day.
There are plenty of promising data points in the battle against a type of breast cancer with a bad diagnosis.
Conclusion
Metronomic treatments are well known and extensively studied for metastatic breast cancer. Low-dose, frequent treatment can add years and increase the quality of life in this diverse disease. In a metastatic setting, weekly doses of cytotoxic drugs have proven efficacy with different side effect profiles. As well, in triple-negative breast cancer, Capecitabine is now a standard approach for early-stage triple-negative breast cancer patients
For more information, contact Dr. Paul Zhang MD at the Omega Precision Oncology, a center for evidence-based cancer treatment.